Glaucoma is a degenerative condition that affects the optic nerve that if left untreated can lead to total blindness in one or both eyes. Many patients with glaucoma have high eye pressure or intraocular pressure (IOP) which is a major risk factor in the development of glaucoma. Glaucoma is one of the leading causes of irreversible blindness in the United States and the second leading cause of blindness worldwide. It is also the leading cause of blindness amongst those of African origin. It is estimated that by the year 2020 there will be nearly 80 million people worldwide with glaucoma and over 11 million blind. In addition, because of the large Asian population, there will be a disproportionate number of Asians with glaucoma. In order to understand what glaucoma is and how it is diagnosed and treated we have presented a short overview of the anatomy of the eye and what goes wrong in the development of glaucoma.
Anatomy of the Eye
The eye is divided into 2 compartments; the front of the eye or anterior segment and the back of the eye or the posterior segment. If you look at the diagram below, you can see that the lens and iris (colored part of the eye) separate the front of the eye from the back of the eye. At the very front of the eye or anterior segment is the cornea and sclera. The cornea is like a window and is the clear part of the eye. The sclera is the “white”of the eye. The lens functions, along with the cornea, to focus light onto the back of the eye. The iris regulates how much light enters the eye by opening or closing the pupil. In the dark, the iris muscle dilates or enlarges the pupil in order to allow more light to enter and help you see better. In contrast, in bright light or sunlight, the iris muscle constricts the pupil to limit how much light gets in the eye.
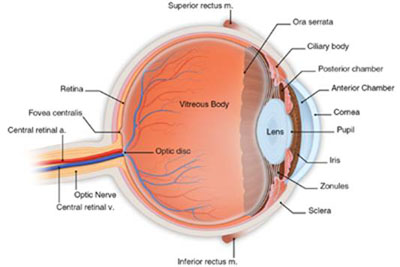
Diagram 1
The front compartment is filled with a liquid called aqueous humor which nourishes and bathes the structures inside the eye that don’t have a blood supply to deliver the nutrition and oxygen needed by these structures. The aqueous humor is also what gives the eye, its shape, form and pressure. The pressure inside the eye is what is known as intraocular pressure or IOP. The normal range of pressure or IOP is between 10-21mmHg. It is important to understand 2 important facts about aqueous humor and eye pressure or IOP. First, IOP has nothing to do with blood pressure. Second, aqueous humor is made inside the eye and should not be confused with tears. Tears are made outside the eye.
Where does aqueous humor come from? Aqueous humor is made inside the eye by the ciliary body which surrounds the lens and is located behind the iris (See Diagrams 1&2). Aqueous humor, once made, circulates around the lens and goes through the pupil and leaves the eye through the internal eye drain called the trabecular meshwork (see diagram 2) which is located in the angle of the eye. This is how nearly 90% of the internal eye liquid or aqueous humor leaves the eye. The rest of the internal eye fluid is absorbed by the iris and ciliary body much like a sponge absorbs water.
Diagram 2
The back compartment or posterior segment is filled with a gel called the vitreous. Sometimes the gel condenses causing floaters that many of you have noticed. The posterior segment also contains the optic nerve and retina. The optic nerve is much like a telephone cable that connects the eye to the brain and consists of a bundle of nerve fibers that work like wires. On the average, there are 1 million nerve fibers bunched together to form the optic nerve in each eye. All visual information from the outside is processed inside the eye by the retina first. The retina is like the “film” in a camera made up of many microscopic layers of cells and supporting tissue and lines the posterior segment like wallpaper. The information processed by the retina in turn is delivered to the optic nerve. The optic nerve then sends the visual messages to the occipital cortex, the visual center of the brain. This is essentially how we see.
What happens in glaucoma?
Many patients with glaucoma have high intraocular pressure (IOP) because the trabecular meshwork and its internal drainage channels don’t work well enough to drain the internal eye fluid or aqueous humor. When the doctor examines the patient he/she can see if the angle is “open” and the trabecular meshwork looks normal but the IOP is high (Diagram 3). The resulting high IOP in turn causes damage to the optic nerve. In such cases the patient is said to have primary open angle glaucoma. In contrast to open angle glaucoma, IOP may be elevated because the angle is closed or narrowed by the iris to a variable
degree. (Diagram 4 and 5) Such patients are said to have primary angle closure glaucoma. Thus, we can see that that there are 2 main types of glaucoma; open angle and closed angle glaucoma.
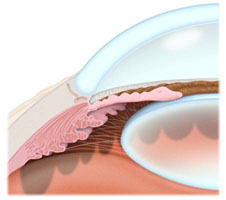
Diagram 3.
Open angle-the space between the iris and cornea is open and the trabecular meshwork is visible
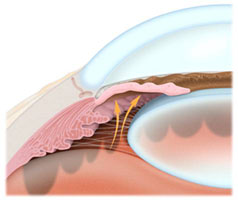
Diagram 4
Narrow angle-in comparison to open angle glaucoma, the iris is pushed up towards the trabecular meshwork narrowing the approach to the trabecular meshwork
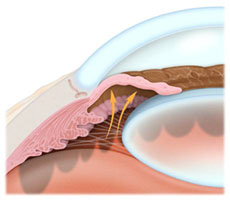
Diagram 5
Closed angle-in this case the iris is pushed up completely into the angle and the trabecular meshwork is not visible
Although high IOP in a susceptible patient causes damage to the optic nerve, not all patients who have high IOP will develop glaucoma. Genetic and racial predisposition, as well as other factors, determines who gets glaucoma. Some patients have glaucoma with normal IOP and have low tension or normal tension glaucoma.
What does the doctor see when the optic nerve is damaged? When the optic nerve becomes injured it becomes hollowed or cupped. Cupping is caused by loss of the nerve fibers or “wires” which connect the eye to the brain. The degree of optic nerve cupping is measured clinically by the cup to disc ratio. Patients with glaucoma who have more advanced cupping or high cup-to-disc ratio (C/D ratio) have worse nerve damage. (see photos 1a, 1b, and 1c).
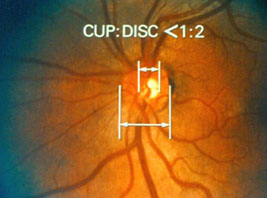
Photo 1 a
This is a photo of the optic nerve head (circular structure with the white center) of a normal eye. One way of determining whether there is glaucoma is to measure the cup/disc ratio or C/D ratio. The cup is the hollow white portion in the center of the optic nerve head. In this normal healthy eye the optic nerve shows a cup that is small relative to the size of the optic nerve head.
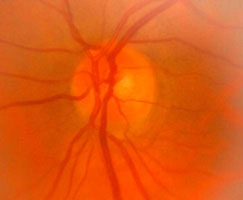
Photo 1b
Healthy optic nerve with normal or small C/D ratio.

Photo 1c
Cupped optic nerve with a very large central cup and high C/D ratio as a result of high IOP
Because the nerve fibers which make up the optic nerve come from cells called ganglion cells that cannot regenerate once these cells die, glaucoma damage is permanent and irreversible. Therefore, loss of vision from glaucoma is likewise permanent and irreversible. Moreover, vision loss from glaucoma is usually slow and affects the periphery, which can go unnoticed by patients. Patients may experience changes in their vision once glaucoma has progressed to affecting their central vision, usually when it has become advanced. For this reason, glaucoma is known as the “silent thief of vision”. Many patients with well established glaucoma have no symptoms or disability but in fact there is irreversible nerve damage that has already occurred. Such patients don’t feel like anything is wrong, but in fact have a very serious problem and peripheral vision testing with the use of a visual field test can often show the injury. There are also sophisticated optic nerve analyzers that can also demonstrate and estimate the degree of nerve fiber loss from the optic nerve very early in the disease process. If the glaucoma is left untreated or inadequately treated the patient eventually loses central vision and eventually all of the vision in one or both eyes.
What is the goal of glaucoma treatment?
The goal of glaucoma treatment is to prevent visual disability and blindness. Because glaucoma, for the most part, is slowly progressive it takes many years for blindness to occur. In some patients, the process of glaucomatous damage is slow enough that significant visual impairment will not occur in their lifetime. However, every patient is individual and the clinical disease course is variable, therefore, one cannot always estimate with reasonable accuracy which patients will or will not be blind or disabled from glaucoma in their lifetime. Also, because glaucoma related vision loss is irreversible and permanent, treatment doesn’t reverse visual loss but only tries to prevent additional visual loss that can lead to disability or blindness.
The treatment plan for glaucoma involves lowering eye pressure or IOP. Even in glaucoma patients in whom IOP starts out in normal range, lowering eye pressure helps prevent the disease from worsening or progressing. Unlike high blood pressure not all patients need the same level of eye pressure or IOP to prevent the disease from progressing. Some patients with more “resistant” optic nerves can tolerate a higher IOP, other patients need much lower IOP. What level of pressure is appropriate depends upon each individual patient’s susceptibility and degree of existing visual loss from glaucoma. The patient’s overall health status, age, and family history of glaucoma also play a role in determining the course of treatment.
How is IOP lowered?
IOP can be lowered in many ways including the use of various eye drop medications, laser, or even surgery. Most commonly, medications and laser are tried first. In patients with uncontrolled or advanced disease filtering surgery is often necessary to control pressure. An evaluation and treatment plan can be tailored specifically to the patient’s needs.